Blood Components
Human blood is a fluid connective tissue that performs multiple essential body functions, including transport, defense, and regulation. Blood transports gases, nutrients, proteins, and waste products. It defends the body against pathogens and forms clots to prevent blood loss. Blood also helps regulate body temperature, maintains the osmotic pressure that keeps fluid in the intravascular space, and stabilizes the body's acid-base balance.
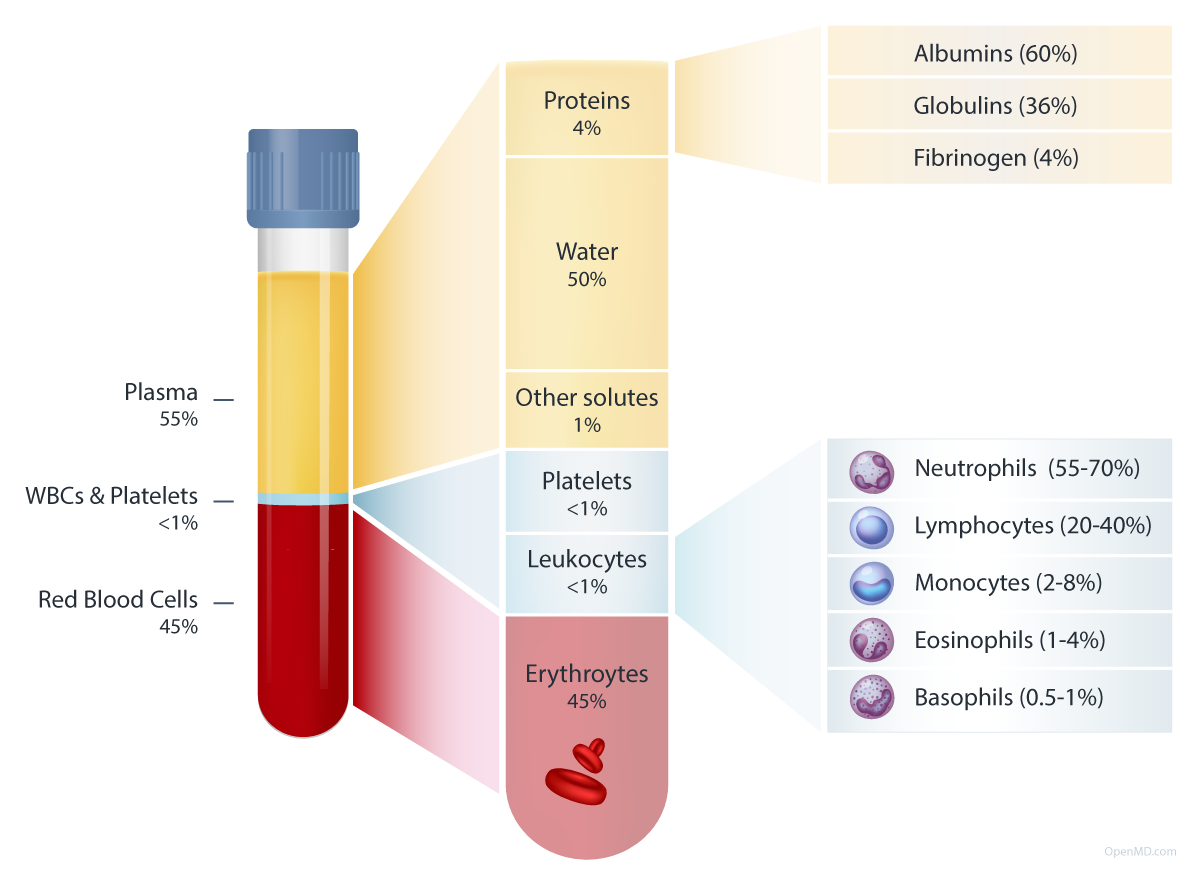
Blood consists of approximately 45% formed elements (red blood cells, white blood cells, and platelets) by volume suspended in 55% liquid plasma. Plasma carries formed elements, proteins, and other substances throughout the body. The cardiovascular, endocrine, digestive, skeletal, and urinary systems all regulate blood composition. The average adult has about 5 liters (1.3 gallons) of blood, or about 7-8% of body weight.
Plasma
Plasma is the pale yellow liquid component of blood that transports formed elements and other substances throughout the body. Plasma is approximately 91% water and 7% proteins by weight, with the remaining 2% composed of electrolytes, gases, nutrients, hormones, and waste products. Most plasma proteins are synthesized in the liver.
The major plasma proteins can be categorized into three groups:
- Albumins: Albumins are the most abundant proteins in blood plasma, making up about 60% of the total protein content. These proteins are produced in the liver and play a crucial role in maintaining osmotic pressure, which is essential for regulating fluid exchange between blood and surrounding tissues. Albumins also act as carriers for hormones, fatty acids, and other molecules and help transport them to their target cells.
- Globulins: Globulins are a diverse group of proteins that can be subclassified into alpha, beta, and gamma globulins. Alpha and beta globulins are produced in the liver and have various functions, including transporting lipids, metals, hormones, and clotting factors. Gamma globulins, also known as immunoglobulins, are produced by the immune system and play a critical role in defending the body against pathogens, toxins, and other foreign substances.
- Fibrinogen: Fibrinogen is a glycoprotein that is synthesized in the liver. It is converted into a fibrous protein called fibrin during the coagulation process. Fibrin forms a mesh-like network that helps to trap platelets and other blood cells to form blood clots.
Plasma contains many other substances, such as electrolytes (sodium, potassium, calcium, magnesium ions, etc.), dissolved gases (oxygen, carbon dioxide, and nitrogen), nutrients (carbohydrates, amino acids, lipids, vitamins, and other trace elements), and metabolic wastes (urea, creatinine, uric acid, and bilirubin).
Red Blood Cells
Red blood cells (erythrocytes) are the most abundant type of blood cell and comprise 45% of blood by volume. Erythrocytes are 7 to 8 µm in diameter and have a flexible biconcave disk shape. This shape increases the cell's surface area, improving its capacity for efficient gas exchange. It also allows the cell to move through the narrowest of capillaries. Mature red blood cells have no nucleus or organelles. They carry hemoglobin, a protein that binds to oxygen and carbon dioxide. Hemoglobin allows red blood cells to carry oxygen from the lungs to body tissues and transport carbon dioxide from body tissues. However, most carbon dioxide is carried to the lungs as bicarbonate ions in blood plasma. There are 4 to 6 million erythrocytes per microliter of blood, and each can transport up to four oxygen molecules.
White Blood Cells
White blood cells (leukocytes) comprise <1% of blood by volume and protect the body from infection. They can be classified by cellular lineage (myeloid or lymphoid progenitor cell type), by the presence of visible granules in the cell cytoplasm (granular or agranular), or by the type of immunity provided (innate or adaptive).
There are five main types of white blood cells, each of which plays a unique role in the body's immune response.
- Neutrophils: Neutrophils (10-14 µm diameter1) are the most abundant type of white blood cell, representing 55-70% of all circulating WBCs.2 They are part of the innate immune system and primarily target bacteria and fungi. They employ a range of mechanisms to kill target cells, including phagocytosis, enzyme release, reactive oxygen species generation, and neutrophil extracellular trap formation. They are characterized by their multi-lobed nuclei and visible granules in their cytoplasm.
- Eosinophils: Eosinophils (1-4% of WBCs; 10-14 µm) are part of the innate immune system and are involved in the immune response to parasitic infections and allergic reactions. They are characterized by their bi-lobed nuclei and visible granules in their cytoplasm that contain enzymes and other molecules essential for their immune functions.
- Basophils: Basophils (0.5-1% of WBCs; 10-12 µm) are part of the innate immune system and are involved in the allergic response. They are characterized by their bi-lobed nuclei and visible cytoplasmic granules. These granules contain histamine and other substances that cause inflammation and other symptoms of an allergic reaction.
- Lymphocytes: Lymphocytes (20-40% of WBCs; 5-17 µm) come from a common lymphoid progenitor. They include B cells, T cells, and natural killer (NK) cells. B cells and T cells are part of the adaptive immune system, while NK cells are part of the innate immune system.
- B cells: B cells are characterized by their single, round nuclei and lack of visible granules in their cytoplasm. B cells produce antibodies that target specific pathogens.
- T cells: T cells mature in the thymus. Upon recognizing a known antigen, cytotoxic T cells (also known as killer T cells) bind to and release cytotoxic molecules into the infected cell’s membrane. Helper T cells activate and coordinate the immune response by releasing cytokines that stimulate other immune cells. Regulatory T cells control the scope of the immune response.
- Natural Killer (NK) cells: NK cells are part of the innate immune system. They play a critical role in killing cancerous and virus-infected cells.
- Monocytes: Monocytes (2-8% of WBCs; 10-24 µm) are part of the innate immune system and are responsible for phagocytosis (engulfing and destroying) of pathogens and old cells or cell fragments. They are characterized by their large size and kidney-shaped nuclei. Monocytes can mature into macrophages or dendritic cells.
Platelets
Platelets (thrombocytes) are small (2-4 µm in diameter), cell fragments that play a vital role in blood clotting and maintaining vascular endothelium. They are activated when a blood vessel is injured and work with other clotting factors to achieve hemostasis (the prevention of blood loss).
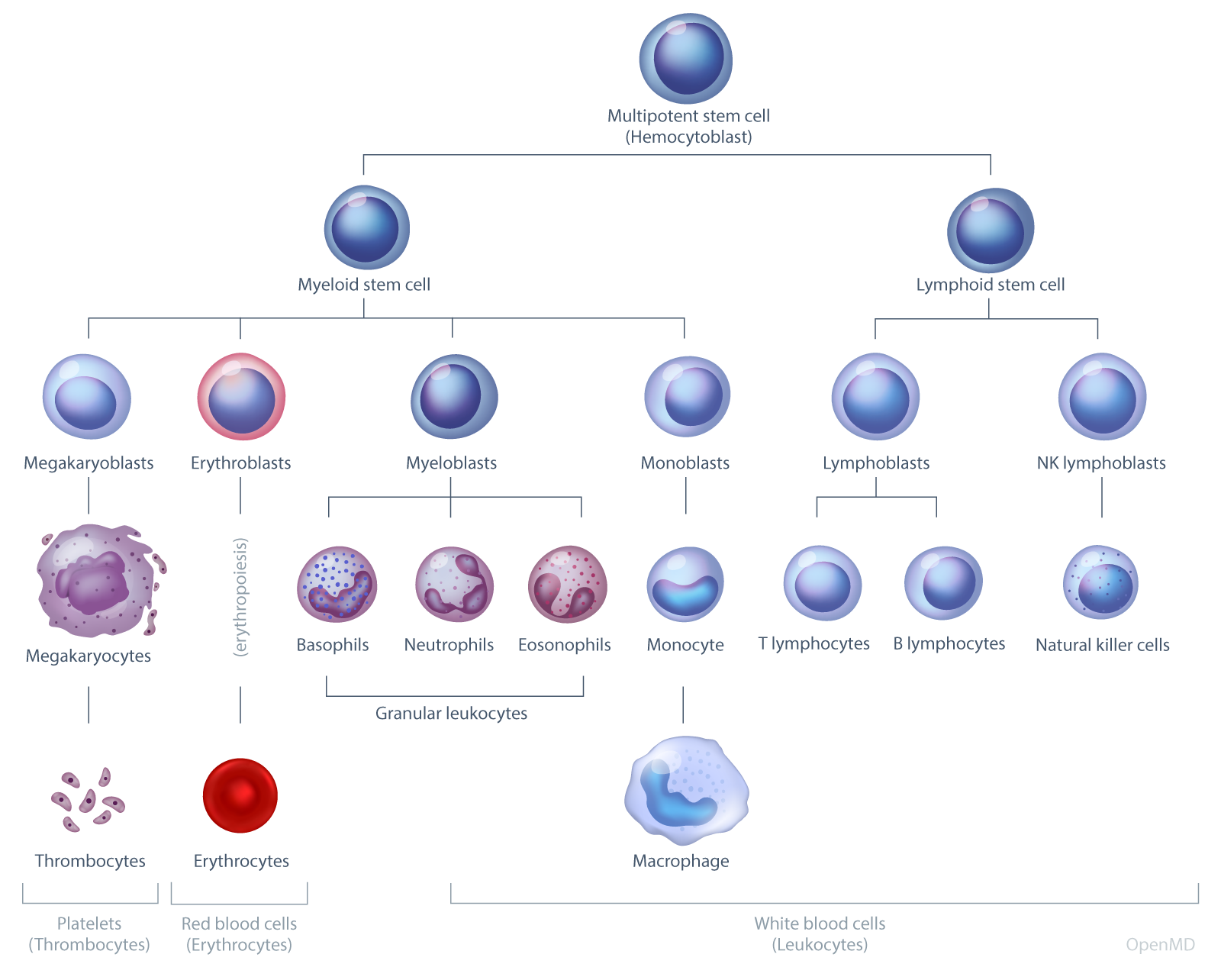
Blood cell development (hematopoiesis) diagram. OpenMD.
Blood Lifecycle
Hematopoiesis is the process by which multipotential hematopoietic stem cells in the bone marrow develop into various types of blood cells. Red blood cells, most white blood cells, and platelets are produced through medullary hematopoiesis in the bone marrow. Some white blood cells, however, differentiate outside the bone marrow through extramedullary hematopoiesis, which primarily occurs in the liver, spleen, thymus, and lymph nodes.
Erythropoiesis is the specific process by which red blood cells are produced in red bone marrow. This process generates approximately 2 million RBCs per second.3 A myeloid progenitor stem cell undergoes several differentiation stages and mitotic divisions to ultimately form orthochromatic erythroblasts. These erythroblasts then eject their nuclei, becoming reticulocytes or immature RBCs, which are subsequently released into the bloodstream and mature into erythrocytes.4
Upon encountering a specific antigen, B cells and T cells undergo rapid proliferation through a process called clonal expansion. This occurs mainly in secondary lymphoid organs, such as lymph nodes and the spleen, where B and T cells come into contact with antigens presented by antigen-presenting cells (APCs). Clonal expansion allows for the generation of a large number of effector cells that can specifically target and eliminate the identified pathogen.
Blood cells have varying lifespans depending on their type: erythrocytes last for approximately 120 days, platelets for 5-9 days, and leukocytes for durations ranging from several hours to years.5, 6
When blood cells become old or non-functional, macrophages engulf and break them down, recycling or eliminating their components. Hemolysis, the destruction of red blood cells, occurs throughout the body but is primarily concentrated in the spleen.
Blood Types
Blood types refer to the different antigens and antibodies found on the surface of red blood cells. The ABO typing system is the most commonly recognized, with blood types A, B, AB, and O. Type A individuals have A antigens on their red blood cells and produce anti-B antibodies. In contrast, Type B individuals have B antigens and produce anti-A antibodies. Type AB individuals have both A and B antigens on their red blood cells and do not make any anti-A or anti-B antibodies. Type O individuals do not have any A or B antigens on their red blood cells but produce both anti-A and anti-B antibodies. The Rhesus (Rh) system is another commonly-used blood typing system. It classifies blood as Rh positive or negative based on the presence or absence of the RhD antigen.
For more information on blood types and donor compatibility, see Blood Types.
Additional resources:
- Components of Blood by Merck Manuals
- Human Blood by Britannica
Contributors:
- Teresa Roberts, DNP
Reviewers:
- Reitze Rodseth MBBS, PhD
References:
- Marieb, E. N., & Hoehn, K.. Human Anatomy & Physiology (11th ed.). Pearson; 2018. [Albumins: 60%; Globulins 36%; Fibrinogen: 4%]
- Pagana KD, Pagana TJ, Pagana TN. Mosby's Diagnostic and Laboratory Test Reference. 15th ed. Mosby; 2021. p. 973.
- Palis J. Primitive and definitive erythropoiesis in mammals. Front Physiol. 2014. https://doi.org/10.3389/fphys.2014.00003
- Moras M, Lefevre SD. From erythroblasts to mature red blood cells: organelle clearance in mammals. Front Physiol. 2017. https://doi.org/10.3389/fphys.2017.01076
- Hoffman R, Benz EJ Jr, Silberstein LE, et al. Hematology: Basic Principles and Practice. 7th ed. Elsevier; 2017. [RBCs 120 days (p447) 3-4 months (p472). Platelets 5-9 days (p1894)].
- Borghans JAM, Tesselaar K, de Boer RJ. Current best estimates for the average lifespans of mouse and human leukocytes: reviewing two decades of deuterium-labeling experiments. Immunol Rev. 2018;285(1):233-248. https://doi.org/10.1111/imr.12693
Published: March 30, 2023